Researchers University of California, San Diego School of Medicine, along with colleagues in The Netherlands and United Kingdom, have constructed a map detailing the genetic reactions underlying the response of cells to ultraviolet radiation (UV) exposure.
It is hoped the study will shed light on the ways in which cells are damaged by radiation and on the mechanisms that repair cells. UV radiation can cause malignancy, especially in skin cancers, and understanding the repair mechanisms may enable scientists to gain more insight into the process of cancer formation.
Some 89 UV-induced functional interactions were studied among 62 protein complexes. These interactions were taken from a larger measurement involving the deletion of two separate genes. Observations were made before and after different doses of UV radiation.
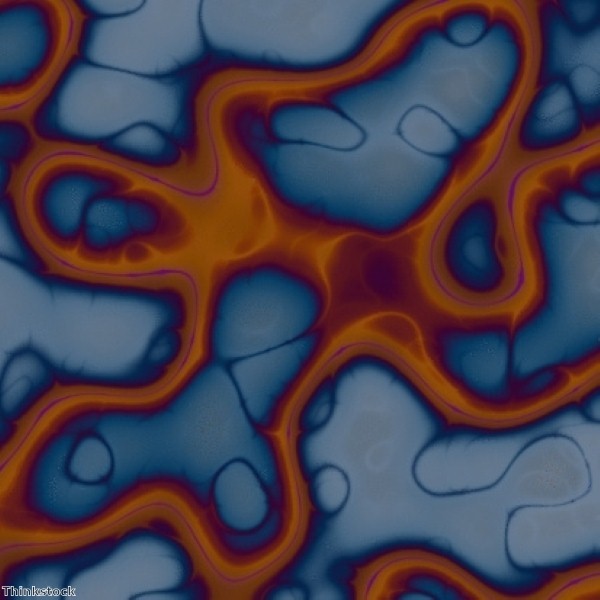
Links were identified between the radiation and the cell's chromatic structure remodelling complex (RSC). Chromatin is a combination of DNA and proteins which forms a cell's nucleus and is remodeled during cell division. According to the researchers, RSC is directed to places on damaged genes and DNA, helping to facilitate effective repair.
The nucleotide excision repair (NER) pathway identifies DNA-distorting lesions and removes them from the genetic material. The gap is then filled with new genetic material copied from an undamaged DNA strand and sealed by an enzyme.
NER works in conjunction with other mechanisms, including RSC.
Dr Rohith Srivas explained that in order to do their job, repair factors need access to undamaged DNA. Chromatin remodelers can be recruited to the DNA and open it up for the repair factors to perform their function.
"Our results are novel because they show RSC is connected to both UV damage pathways: transcription coupled repair – which acts on parts of DNA being expressed – and global genome repair, which acts everywhere. All previous remodelers were linked only to global genome repair," Dr Srivas commented.
The scientists observed that the degree of genetic rewiring is correlated with the dose of UV. Reparative interactions were observed at distinct high or low doses of UV.